Abstract
Introduction
Monoclonal gammopathy of clinical significance (MGCS) is a newly described entity that defines clinical conditions and organ damage resulting from the effects of monoclonal proteins (Fermand et al., 2018). In MGCS, the underlying clone burden resembles an MGUS state, and does not meet criteria for multiple myeloma or lymphoma. A wide spectrum of conditions has been described in MGCS (Fermand et al., 2018). In this retrospective study, our purpose was to identify the incidences of patients with MGCS at our hematology clinics.
Methods
We collaborated with three clinicians who see the majority of MGUS patients at the University of Calgary Medical Group clinics (UCMG). Patients who were referred and diagnosed with MGUS at the hematology clinic at UCMG since 2014 were assessed. The diagnosis of MGUS and MGCS were made based on consensus criteria (Rajkumar et al., 2014) and the recent publication (Fermand et al., 2018). Retrospective chart reviews were performed and cases with MGCS were analyzed. MGUS risk stratification score was calculated per previous reports (Katzmann et al., 2013; Kyle et al., 2018). Hematological response was assessed using the International Myeloma Working Group criteria (Rajkumar et al., 2014), and renal response was measured using KDIGO guidelines (Radhakrishnan & Cattran, 2012).
Results
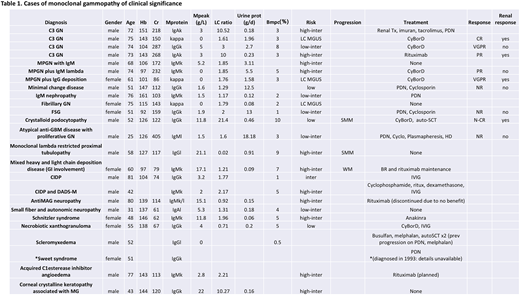
A total of 606 MGUS patients were seen at our clinic from February 2014 to June 2018. Patients who had MGUS and co-existing conditions which met MGCS criteria (Fermand et al., 2018) were evaluated. There were 25 MGCS patients identified. Median age at diagnosis was 60, and 28% were female. Clinical characteristics are outlined in Table 1. Three patients had light chain MGUS. Among the non-light chain MGUS patients, there were 11 high-intermediate risk (55%), 1 intermediate risk (5%), 5 low-intermediate risk (25%), and 3 low risk MGUS (15%). At the time of analysis all patients were alive, and 3 patients have progressed. Median follow up was 2 years (0-16 years).
Renal involvement was the most common with 14 patients having biopsy proven renal pathologies that met criteria for monoclonal gammopathy of renal significance (MGRS) (Leung et al., 2012). Four patients had neuropathies, including Anti-MAG, chronic inflammatory demyelinating polyneuropathy (CIDP), distal acquired demyelinating symmetric neuropathy (DADS-M), and autonomic neuropathy. Three patients had skin manifestations (Schnitzler syndrome, necrobiotic xanthogranuloma, scleromyxedema), 1 patient had corneal involvement (crystalline keratopathy), 1 patient had gastrointestinal manifestation (mixed light chain deposition disease), 1 patient had acquired C1 esterase inhibitor deficiency with angioedema, and 1 patient was diagnosed with Sweet syndrome in 1993 which had led to her original monoclonal gammopathy workup.
Five out of the 14 patients with MGRS received plasma cell directed chemotherapy, and 1 patient with crystalloid podocytopathy underwent auto-stem cell transplant. Of these 5 patients, 4 had renal response. Treatment for other MGCS cases are indicated in Table 1.
Discussion and Conclusion
Our series demonstrates that cases of MGCS represent a small minority within our larger MGUS cohort. The most common organ involvements seen in our MGCS patients were renal, nerve and skin. One of the major diagnostic challenges is confirming that the organ dysfunction and MGUS co-exist by true association, and not by coincidence. In our patient cohort, tissue biopsies were obtained when possible (all renal, skin, and GI cases), and others were diagnosed through review with local experts and relying on published literature.
The distinction of MGCS from MGUS is important, as it may change treatment decisions. In renal diseases associated with monoclonal gammopathy, referred to as MGRS, renal prognosis is poor and clone directed treatment is associated with improved renal outcomes (Fermand et al., 2013). As prospective or randomized trials are unavailable for MGRS or MGCS, the treatments given at our center were determined on a case-by-case basis relying on expert opinions, local experiences, and a recent guideline (Fermand et al., 2013). Interdisciplinary care is required for both the diagnosis and management of MGCS. Further studies with long term follow-up are needed.
McCulloch:Takeda: Other: Travel expenses; Celgene: Honoraria. Neri:Janssen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal